Scientists Develop Personalized Anti-Cancer Vaccine That Works in Mice
A research team in Montreal has been busy developing a personalized cancer vaccine that works in mice.
At the Research Center of the University of Montreal Hospital (CRCHUM), Marie-Claude Bourgeois-Daigneault and a team of scientists modify viruses to make them specific to tumor cells.
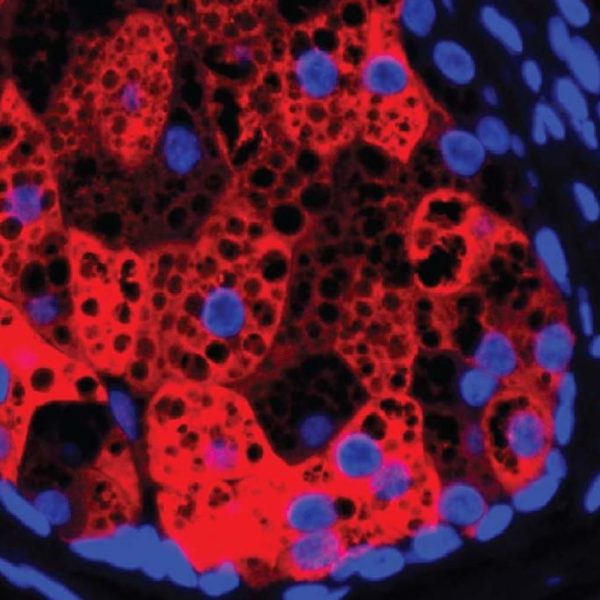
Once in the patient’s body, these viruses, called oncolytic viruses, specifically infect and destroy cancer cells without touching healthy cells. These viruses can even stimulate the immune system so that it is better armed to recognize and kill malignant cells. This is what is known as immunotherapy.
In a study published in Nature, the researchers show how they came to create an effective personalized vaccine by combining oncolytic viruses with small synthetic molecules (peptides) specific to the target cancer.
Here, Bourgeois-Daigneault explains his team’s approach and findings.
In his study, he uses oncolytic viruses as cancer vaccine adjuvants to immunize mice. How do you do it?

For a vaccine to induce an immune response, it must contain elements that stimulate the cells of the immune system: the famous white blood cells.
These elements, called adjuvants, are ingredients in all vaccines. They allow the human body to perceive the potential danger and contain the threat by dispatching its army of immune cells.
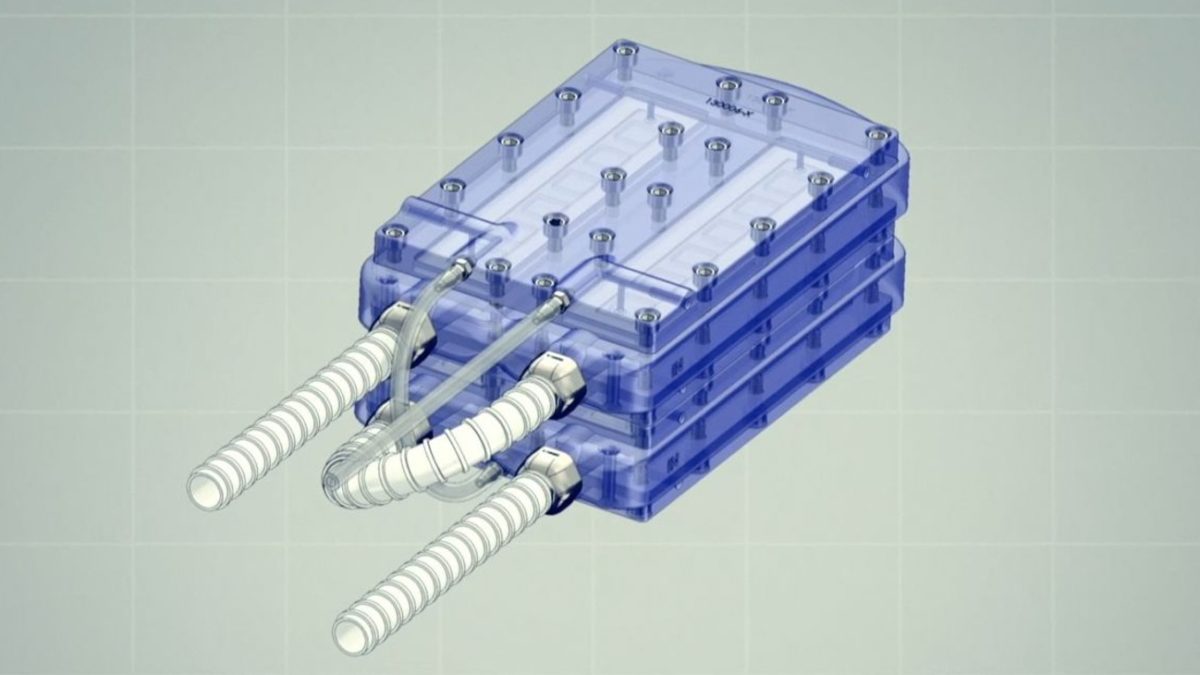
Our approach is to use oncolytic viruses to stimulate this immune response and target it to cancer. To be successful, we created a vaccine by mixing viruses with synthetic peptides (antigens) that resemble the target cancer.
Because it is true that, to be effective, the vaccine must be personalized for each patient, based on the specific mutations of each cancer cell. Thanks to the identification work carried out by other research teams, we can predict which peptides to use for each patient through the information obtained from a biopsy.
The advantage of our approach is that the oncolytic viruses themselves have the power to kill cancer. Thus we can attack cancer on two fronts: kill it directly with the virus and induce an immune response, thanks not only to the virus, but also to the vaccine.
In our mice, we were able to demonstrate the efficacy of the resulting immunization.
What distinguishes your vaccination strategy from the clinical trials currently being conducted by other teams?
The other clinically proven personalized cancer vaccines do not use oncolytic viruses as vaccination adjuvants. Therefore, its adjuvant does not have direct anticancer effects whereas, in our case, our viruses can destroy cancer.
A cancer vaccine using oncolytic viruses is currently being tested in Canada and the United States. However, it is not personalized. Instead, it targets certain specific cancers that have an antigen in common. By targeting this antigen, the vaccine induces an immune response.
In this case, the oncolytic viruses must be genetically modified to allow insertion of the antigen into the genome of the viruses.
CHECK: Green Tea Compound Could Be Key To Beating Cancer, Says Compelling New Study From ‘EGCG’
This is very different from our approach. We can target all cancers without genetic modification. A bit like building Lego: it’s about mixing synthetic peptides that resemble cancer with the chosen virus. It will be much easier to implement in a clinical setting.
What challenges need to be addressed before your personalized approach to cancer vaccination can be translated into clinical practice?
The main challenge is to identify the mutations against which we want to be vaccinated. Because a cancer is unique in its tens or hundreds of mutations, but only some of them, once targeted, will have a therapeutic effect and allow us to eliminate it.
MORE: Researchers create CRISPR ‘on-off switch’ to control inherited genetic problems without changing DNA
Identifying these mutations is the key step that still needs to be optimized. Fortunately, many groups are working in this area.
Source: University of Montreal; Featured Image: Dodgerton Skillhause, CC License
SHARE this hopeful breakthrough with others on social media …